- Disc (think of the 3 Cs: cup, colour and contour)
- macula
- Vessels
- Periphery
- Vitreous
- if nil abnormal seen, go through repeat systematic examination
- if still nothing seen, ask if you can use indirect?
- if an abnormality found, look for another!
| 1. Use your
own ophthalmoscope.
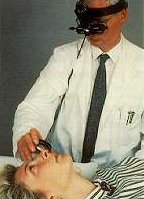
2. Observe the patient for any abnormal physical signs. 3. Dim the light to give better contrast. 4. Ask patient to fixate on distance object. 5. Do not block vision to fellow eye. 6. Quickly look from 10 cm with plus for red reflex and anterior segment. 7. Examine structures in a methodical sequence, with commentary
(if required).
Indirect Ophthalmoscopy 1. Check equipment to obtain binocular view before the examination. 2. Look at fundus in logical order (see above).
In most cases, the patients would have their pupils dilated. In patient whose pupils are not dilated, the examination is usually confined to the optic disc. The best way to prepare for retinal examination is to : 1. anticipate the type of lesions you may see. for example in the optic disc the most likely lesions would be optic atrophy, optic coloboma, optic disc pit, glaucomatous disc, optic disc drusen and neovascularisation of the disc etc
for example in the case of optic disc pit look for any pigmentary macular changes which may suggest previous central serous retinopathy, optic disc drusen may have associated angioid streaks or retinitis pigmentosa
|
||||
| Back to the index for final MRCOphth |