Date: Nov., 2001
![]()
Mostly based on Optics , instruments, optics, MRI, and optics again! very
few clinical ophthalmology questions!
0SE
1) Fluorescein angiogram: CSR but with no smoke-stack and no clear hot spot.
This question was longish, as we should also illustrate the principles of
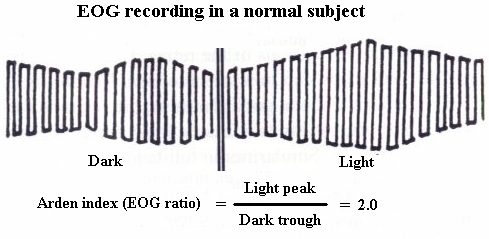
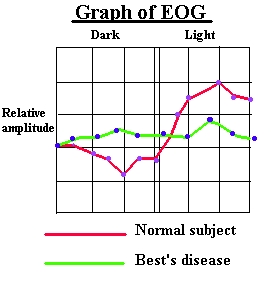
FFA.2) EOG- normal patient. This station created havoc, as many of us never saw
an EOG (me included). But the clue was the Arden ratio printed at the
bottom. Therefore, in future, just do not panic and keep your eyes wide
open...
|
 |
OSCE
3) A list of visual acuity tests for children and three examples. Like :
which test is more appropriate for a child of 6 months? etc. A piece of
cake.4) Visual field (humphrey). Right incongrous scotoma, left relative scotoma.
Some people defined it as an early bitemporal scotoma, I simply wrote that
the lesion was in the anterior chiasm. Once again, we were asked to
localize the lesion, NOT to make a diagnosis!5) CT scan. Thyroid eye disease. Another piece of cake.
6) B scan with A scan at the bottom of the page. Looked like a mushroom
shaped choroidal melanoma. Again, no diagnosis required, we were just asked
to name the structures involved.7) A tonometer head was given. We were asked to draw the related diagram. A
lot of people drew the two half circles but the right diagram was the one
on the Elkington-Frank, with the cornea being flattened , the pressure from
the tono-head..come on you know it!8) Hess chart. Dodgy one, looked like a sixth nerve palsy but no sequelae
and a vertically restricted field. As no diagnosis was asked, I decided
just to describe which muscle was overacting/underacting, evidence of
sequelae etc.I was pleased that there were no dodgy Ray diagrams to draw!
1) Goldmann perimetry. We were asked to set up the instrument.aargh.Refraction2) Ocular motility. I had a nice girl of 5 that was reasonably cooperative
and had fully accomodative esotropia. I know of other candidates that were
not able to perform anything as the young patient was bored or not
cooperative.3) Focimetry. I was asked to write the prescription of a lens (bifocal), to
transpose it, plus few more questions about the optics of the focimeter.4) Keratometry (javal schiotz). Normal cornea. After the measurement, again
a lot of questions about the optics of the instrument.5) Direct ophthalmoscopy. Here I honestly made a mess, as I forgot the
+10D on and I kept repeating the examiners that i could not see nothing!
When I realized it, I had time to give just a look at the disc (OK) and the
macula (drusen). Some other candidate saw a haemorrhage, another a
mulberry-like lesion.6) Indirect ophthalmoscopy. Tiny area of retinoschisis. The patient was
sitting on those flashy reclinable chairs, but she was quite low (almost on
the floor). at the end, they asked me about the differences between 20 D
and 28D lenses.7) Pupils. The most classical case of Horner's syndrome.
8) Slit lamp. A young lady with ?corneal dystrophy. They wanted me to say
whether it was epithelial, stromal or endothelial and asked me to show how
I do scleral scatter and specular reflection.In all stations, whenever a machine was involved (slit lamp, indirect,
focimeter) I carefully checked all the knobs and oculars etc. Usually they
were out of range.
I was lucky enough, to have a lady with +6.75/-0.50 and +7/-0.75. But I
know that some of us had to refract a corneal graft, amblyopes etc while
some others had nurses and clerical staff from that department that were
emmetropes! as you see, a bit of luck is always needed!
| More experience |