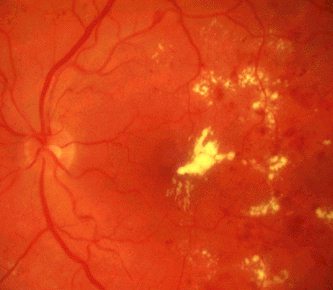
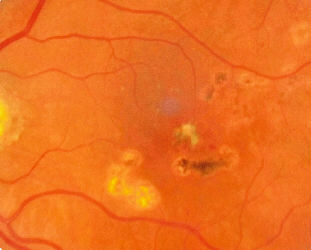
Diabetic maculopathy
|
||
| Note: This is a very popular case, you must demonstrate
to the examiner(s) that you know what is meant
by significantly macular oedema (this is done through physical examination and not fluorescein angiography). The maculopathy may occur in background diabetic retinopathy or in association with preproliferative or proliferative diabetic retinopathy. The clinical appearance of the maculopathy alone cannot distinguish between ischaemic from non-ischaemic maculopathy. There are multiple dot and blot haemorrhages, microaneurysms
and hard exudates (which may be circinate and
a. retinal thickening at or within 500um of the centre of the macula |
Questions:
1. What is the most common cause of visual loss in diabetic
retinopathy?