Cataract
|
||||||
|
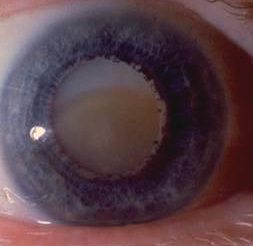
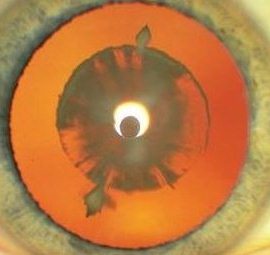
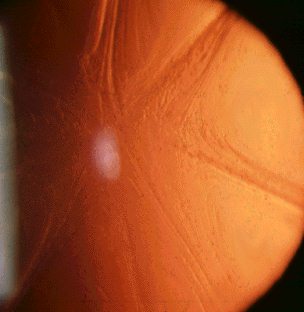
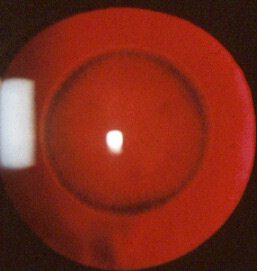
Cataract may be cortical, nuclear, subcapsular or in any combination. Examine the cataract with different forms of biomicroscopic illumination so that you can describe the location of the cataract. For example, retroillumination is best for anterior and posterior subcapsular opacities whereas direct focal slit illumination is best for examining the different zones of the lens and thus locate the opacities. The location of the cataract can suggest the cause. In the examination:
relaxation) |
Questions:
1. What happen to the lens in poorly controlled diabetes
mellitus?Answer
2. In which form of cataract would the patient gain a second sight and why?